Key Takeaways on FMTs in the Treatment of CDI
Experts provide practice pearls for educating patients on and using FMTs for the management of CDI.
Episodes in this series

Stuart Johnson, MD: Joseph, do you have any final thoughts about, or takeaways from, this discussion?
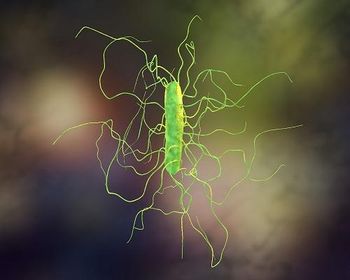
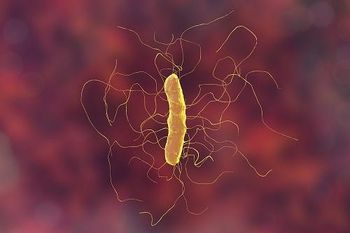
Joseph Reilly, BS, PharmD, BCGP: Education is important for everybody. Many health care providers, including myself, always had this feeling about FMT [fecal microbiota transplant]. Is it dangerous? Will patients wind up getting sick? Where does the stool come from? Is it a mix of donors or a single donor? How much will it cost? And the whole idea of a colonoscopy with bowel prep and propofol, which I mentioned before, seems like a lot. We need to change the way we think about the natural course of Clostridioides difficile infection [CDI]. Hopefully, people will and explore all treatment options that are available at this point.
Stuart Johnson, MD: Thank you. Candace?
Candace Cotto, RN: As far as education with the practitioners, it is about educating the patients as well. If they happen to be frequent fliers for, let’s say, as you mentioned, UTIs [urinary tract infections]. Or they go to their physician, and they say, “I have a cold,” and they’re given an antibiotic. You have to explain to patients as you’re seeing them come into your practice that it’s not important to get an antibiotic every time you go to your physician’s office. And to educate them and not to try to doctor-shop and get an antibiotic if they don’t get the right answer from their primary care physician [PCP] or whomever. It’s important not only for practitioners, but for patients or potential patients for C diff as well.
Stuart Johnson, MD: Certainly, we’re going to continue to need patient education, and I appreciate that comment. Andrew?
Andrew Skinner, MD: I am cautiously optimistic now, at this point, as to where we’re headed with CDI treatment, as we have the first FDA-approved FMT product at this point right now with seemingly more on the way. We’ve got the first one through the door, and it’s going to be a matter of seeing where things go from here. As you mentioned earlier, maybe hopefully in the next 10 years we’ll have narrowed it down to which key microorganisms are essential for restoring the microbiota. And if we see these improvements, then hopefully the treatments will continue to become more effective into the future as well.
Stuart Johnson, MD: Appreciate that. I have to say that I’ve considered myself in the past a drug pusher, if you will, in the good sense of the term. But I am excited the fact that there is now an FDA-approved fecal microbiota replacement and that’s a nice, good step forward with assurance that it’s screened and safe, for the most part. And that’s a major step for managing patients with recurrent C diff. Thank you for watching this HCPLive® Peer Exchange. If you enjoyed the content, please subscribe for e-newsletters to receive upcoming Peer Exchanges and other great content right in your inbox.
Transcript edited for clarity
Newsletter
Stay ahead of emerging infectious disease threats with expert insights and breaking research. Subscribe now to get updates delivered straight to your inbox.