Economic Implications of FMTs on CDI
Joseph Reilly, BS, PharmD, BCGP, reviews the positive economic impact of use of live-jslm for treatment of CDI in a hospital setting.
Episodes in this series

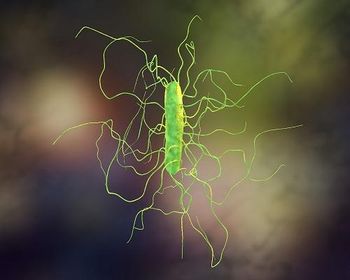
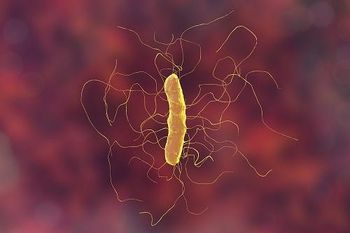
Joseph Reilly, BS, PharmD, BCGP: When patients come in the hospital with Clostridioides difficile, there are certainly a lot of economic considerations in this population. We did a study at our hospital looking at recurrent C diff. Patients who were admitted at least 3 times. Think about this, just 3 times with the admitting diagnosis being C diff infection [CDI], and we found over a couple-year period that we had 29 patients who were frequent fliers. They had come in our hospital a minimum of 3 times with C diff and kept coming back. And what we found among 29 patients, we did an economic analysis, and we found that it cost us over $2 million to treat these patients. Even with reimbursement in every case, we still lost about $1.4 million or more in this patient population. The same 29 patients. So the economics—and this is coming from…a nonprofit teaching hospital. We really have to think about this. There was a great economic impact in a small number of patients, and it makes us keep an open mind as far as what our treatment options are in these patients. In the case of the new FDA-approved live fecal microbiota suspension [live-jslm], we could be reimbursed for the product more than we paid for it and prevent future admissions to the hospital for C diff,and change the outcome of a patient’s life. The big-picture view of utilizing this new treatment is very promising for us, both economically and from a patient quality of life standard.
Stuart Johnson, MD: Sounds like a win-win. I have to say your hospital is exemplary, and looking at the big picture, I would say that not all hospitals are like that. Again, it may be a struggle. I assume you have to have this put on your pharmacy and therapeutics [P&T] committee, that it has to be approved?
Joseph Reilly, BS, PharmD, BCGP: We approved the product through our P&T, and the initiative, the push, is to improve our antimicrobial stewardship program, to lower our C diff rates, and to create initiatives that are economically beneficial for our hospital, which is once you start saying that we can save a lot of money and improve patients’ lives, it gets the attention of administration in a hospital. So our financial analysts will take a look at the whole process and decide that this is a win-win for the hospital.
Stuart Johnson, MD: That’s great. I know traditionally, Medicare reimbursement has been linked to readmission in 30 days, not necessarily for C diff. And then C diff rates, per se, are determined by a calculation on what kind of testing you’re doing, what the facility is. So if your rates are high, you can get dinged for that. But so far, they haven’t talked about readmission specifically for C diff infection, which I appreciate you bringing it up because we’ve seen this ourselves. This is a major issue, and we have a referral clinic for C diff patients in our hospital. We’ve thought about making a more mandatory follow-up for patients who are seen with C diff in the hospital; as you know, patients can show up on the orthopedic ward. They can show up on the surgical ward, etc. And they’re handled by their own practitioners, per se, and the follow-up they get may not necessarily be appropriate. They may be given a prescription and told to call back if they have a problem. We think we could do better than this. And if we have a dedicated clinic where patients are funneled to this, they may not need a lot of handholding but at least referral for a call if need be. That’s something that should be thought about more in institutions.
Joseph Reilly, BS, PharmD, BCGP: Imagine a scenario where you have a patient who has their third episode of C diff; their second recurrence. Knowing what we know now, with an FDA-approved product, what are the chances of that patient coming back within the next 60 days and being admitted to the hospital, possibly with C diff? According to studies, it’s 50% or greater. So how can we not at least have a discussion with this patient that there’s an FDA-approved product out there that is effective?
Stuart Johnson, MD: I would have to say that nothing is 100%. And that patient selection for this is a big issue and that a patient who has recurring urinary tract infections [UTI], a neurogenic bladder, who gets treated for a UTI every month or so might not be the ideal patient in whom to initiate this therapy. That would be my perspective. But there are a lot of issues with this. This is clearly an effective treatment for many patients. Patient selection, however, is going to be important, and certainly this issue of asymptomatic carriage and misidentifying patients who may be colonized but not necessarily have infection due to C diff, meaning they have a positive polymerase chain reaction [PCR] but yet they hadn’t been on antibiotics recently. They hadn’t been in the hospital, and they don’t respond to vancomycin or fidaxomicin. I don’t think we can expect them to respond to the FMT [fecal microbiota transplant], if you will. It’s probably a misdiagnosis. So careful patient selection for this is going to be important.
Transcript edited for clarity
Newsletter
Stay ahead of emerging infectious disease threats with expert insights and breaking research. Subscribe now to get updates delivered straight to your inbox.