C Difficile Infection: The Importance of the Gut Microbiome
Opening their discussion on Clostridioides difficile, experts provide an overview on the gut microbiome and colonization resistance.
Episodes in this series

Transcript:
James A. McKinnell, MD: Hello, and welcome to this HCPLive® Contagion® Peer Exchange titled “The Relationship Between the Gut Microbiome and Management of C Difficile.” I’m Dr Jamie McKinnell, from the Lundquist Institute at Harbor–UCLA Medical Center [in Los Angeles, California]. Joining me in this discussion are my colleagues Dr Carl Crawford, an assistant professor of clinical medicine at Weill Cornell Medical College in New York; Dr Sahil Khanna, a professor of medicine at the Mayo Clinic in Rochester, Minnesota; and Dr Kelly Reveles, an assistant professor at The University of Texas at Austin College of Pharmacy.In this discussion, we’re going to investigate the role between the microbiome and Clostridium difficile [C difficile]. It starts logically by establishing the role of the gut microbiome and the impact of dysbiosis in health care.
For the first question, I’ll turn to you, Carl. What’s the gut microbiome, and what does it consist of?
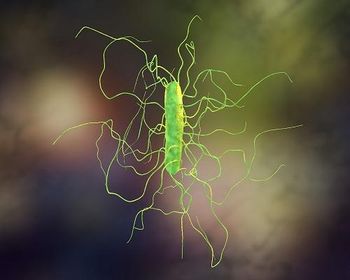
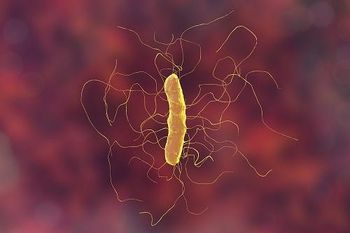
Carl V. Crawford, MD: That’s an easy and a complex answer at the same time. Microbiota refers to the collection of all the bacteria that are inside the human organism. If we think about how it pertains to C difficile infections, we can focus on the microbiota of the gastrointestinal tract. Microbiome refers to all those bacteria and organisms as well as their genomes. We tend to use them interchangeably. We may say microbiota to refer to the bacteria, and we also use the term microbiome, so it’s important to make a distinction between the 2. But for the most part, we’ll use microbiome in this discussion.
The microbiome or the microbiota are impressive. Inside the gastrointestinal tract, there are 100 trillion kinds of organisms floating around and out of those and more than 35,000 bacterial species. These bacterial species will fit into certain kinds of phyla, with firmicutes and bacteroidetes being the 2 major phyla. There are several other phyla as well, into which almost 90% will fit into most of those bacteria. That’s just bacteria that we’re talking about, but we have to also remember all of the other kinds of organisms that live with inside of the gastrointestinal tract, such as yeast, fungi, protozoa, fungi, and so forth, as well as the viruses. It’s pretty impressive when we talk about the microbiome because we’re referring to everything that’s inside the gastrointestinal tract.
James A. McKinnell, MD: It’s almost like a forest of different organisms. There are lots of different components in there. Is there a function of this stuff? Is there a purpose to having this?
Sahil Khanna, MBBS, MS: There are a lot of functions. Back in the day, we were thinking that these microbes might just be pathogens. They’re causing human disease. But over the last decade or 2, we’ve understood that these microbes have a 2-way symbiotic relationship with the human body. There’s a lot of function out there, not only from digestion but from production of lots of vitamins and short-chain fatty acids the body needs, harnessing energy from different components of food that we can digest ourselves. From that to immune regulation, we understand that these microbes are not just sitting inert in our bodies but constantly interacting with the lining of the colon, leading to systemic and local immune regulation and prevention of autoimmune diseases. More important, colonization resistance, is a big function of the gut microbiome. If you have a healthy, diverse microbiome, you have a property called colonization resistance, meaning this gut garden or Amazon rain forest that lives inside your large and your small intestine does not allow colonization and infection from other pathogenic organisms, notably C difficile infection. We see this as a big problem as this colonization resistance goes down.
James A. McKinnell, MD: Let me make sure I’m understanding this correctly. This Amazon or garden that we’re talking about will help you with digestion? So the organisms will help break down the food we eat. Is that making sense?
Carl V. Crawford, MD: That’s correct.
James A. McKinnell, MD: Not only that, but the healthy garden helps your immune system regulate what’s happening in the gut, keeps things stabilized like a healthy garden would. Explain to me more about this invasion of other bacteria like this. For lack of a simple term, C difficile is the bad bug that you chose to talk about. How does that work? How does that impact things? What’s the protection mechanism?
Sahil Khanna, MBBS, MS: In simple terms, when you have a complex gut microbiome or a diverse gut microbiome, they have functions, what we call complex metabolism. They interact with one another, produce lots of mediators, and help convert some of the primary bile acids in our body to secondary bile acids. When you disrupt this balance of gut microbiome with risk factors like antibiotics and hospitalizations; uncontrollable risk factors, like age over 65; or other comorbid conditions, which we’ll go into later in our discussion, then the complex metabolism goes into what we call simple metabolism. The diversity goes down, the metabolism goes down, and the number of metabolites that they produce goes down. There is less conversion from primary to secondary bile acids. In simple terms, C difficile finds an empty home where it can germinate from the spore form to the vegetative form and cause disease.
James A. McKinnell, MD: Kelly, I’ll turn to you on this 1. When we’re looking at the structure of this garden in the intestines, is there a way to describe that or explain how that would help protect you from these sorts of things? Is there a structure that can help us understand that concept?
Kelly R. Reveles, PharmD, PhD, BCPS: Yes, absolutely. We’ve had several very large-scale projects that have attempted to identify what constitutes a healthy microbiome, and it’s not that simple. Some projects, like the human microbiome project, took samples from healthy volunteers to describe what diversity and what community structure is associated with health. What they found is very interesting. We have variability in our microbiome across individuals, and no 2 microbiomes are the same. It’s like a fingerprint. We see the core microbiome mostly maintained across humans, but there’s significant variability, especially at the lower taxonomic levels.
What constitutes a healthy microbiome is a hard question to answer. Scientists have proposed several factors that would make a healthy microbiome. One is having a core structure that’s going to provide all the housekeeping genes and the production of compounds that are necessary to support human life. The next is having high microbial diversity. That typically refers to the total number of bacterial taxa within the ecosystem. With increased diversity, you have increased functional capacity and functional redundancy. If you lose some beneficial microbes, you still maintain that core function. The last marker of health is stability and resilience of the microbiome, which refers to the ability of the microbiome to recover once it’s been disrupted. Those are our core components of what constitutes a healthy microbiome.
James A. McKinnell, MD: Thank you for watching this HCP Live® Contagion® Peer Exchange. If you enjoyed the content, please subscribe to our e-newsletters to receive upcoming Peer Exchanges and other great content right in your in-box.
Transcript edited for clarity.
Newsletter
Stay ahead of emerging infectious disease threats with expert insights and breaking research. Subscribe now to get updates delivered straight to your inbox.