Hospital Exposure to Antibiotics Associated with C diff Pose Higher Risk of MDRO
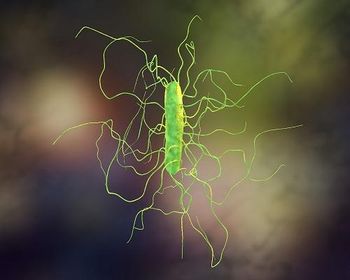
Hospital exposure to antibiotics associated with Clostridioides difficile were linked to a greater risk of multidrug-resistant organisms (MDRO) in nursing home patients and environments, according to research presented during IDWeek 2020.
A team of investigators from the University of Michigan set out to examine the effects of hospital-based antimicrobial stewardship programs on nursing homes. Those involved in the research included Kyle Gontjes, MPH; Kristen Gibson, MPH; Bonnie Lansing, LPN; Karen Jones, MPH, RN, CIC; Marco Cassone, MD, PhD; Joyce Wang, PhD; John Mills, MD; Lona Mody, MD, MS; and Payal Patel, MD, MPH.
“Exposure to high-risk ‘C. diffogenic’ antibiotics, those that markedly increase the risk of Clostridioides difficile infection in the hospital, led to the recovery of multidrug-resistant organisms in nursing home patients and their environment,” the authors told Contagion®. “Therefore, treatments given in the hospital have a downstream impact on patients and their environment in the nursing home.”
The study included 618 post-acute care patients in 6 nursing homes between 2013 and 2016. Patients and high-touch surfaces were screened for methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant enterococci (VRE), and resistant Gram-negative bacilli (rGNB). Results were analyzed to determine whether hospital exposure to C. diffogenic agents — fluoroquinolones, third- and forth-generation cephalosporins, penicillin combinations, lincosamides, and carbapenems — was an independent risk factor for MDRO.
“Antibiotic exposure prior to nursing home arrival was common in our post-acute care patient population,” the authors said. “We identified that approximately 60% post-acute care patients had an antibiotic exposure prior to study enrollment upon arrival to the nursing home. Interestingly, when looking at the types of antibiotics prescribed to these patients, we identified that approximately 66% of these patients received an antibiotic that may have placed them at an increased risk of Clostridioides difficile infection.”
MDRO patient colonization was identified on 350 patients (56.6%), including 98 with MRSA, 208 with VRE; and 196 with rGNB. MDRO contamination was present in 68% of patient rooms, including 166 with MRSA, 293 with VRE, and 182 with rGNB.
Hospital exposure to C. diffogenic antibiotics was an independent risk factor for MDRO patient colonization (OR, 1.94; 95% CI, 1.35-2.79) and MDRO environment contamination (OR, 1.94; 95% CI, 1.43-2.63), VRE patient colonization (OR, 4.23; 95% CI, 2.59-6.90), and VRE environment contamination (OR, 2.58; 95% CI, 2.00-3.33), the study found.
“Clinicians and health care providers should be aware that antibiotic prescribing during the patient’s hospital stay can have a long-term impact on their health, including during their nursing home stay,” the authors said. “Additionally, hospital antibiotic prescribing can indirectly influence the patterns of multidrug-resistant organisms in nursing homes.
“Globally, our data supports investigating the potential value of migrating from being siloed, independent actors in antimicrobial stewardship to forming integrated stewardship partnerships between hospitals and their preferred nursing homes.”
More research is needed to better understand how hospital and nursing home antibiotic exposures affect MDROs and whether antimicrobial stewardship program interventions may influence outcomes.
Earlier this year, the CDC released
More than 2.8 million antibiotic-resistant infections occur in the United States each year, and more than 35,000 people die as a result.
Newsletter
Stay ahead of emerging infectious disease threats with expert insights and breaking research. Subscribe now to get updates delivered straight to your inbox.